My Type 1 Diabetes Diagnosis Story
In the Type 1 Diabetes world, those of us with T1D commonly share our diagnosis stories. Everyone has a different narrative, partly because type 1 develops differently in each person. To the individual, it may seem as if Type 1 Diabetes comes on suddenly – in a matter of days or weeks, but science suggests 1 that Type 1 diabetes often has a protracted development phase before you notice overt symptoms. Many people who received their diagnosis as children report that symptoms came on suddenly – often in a matter of days. For me, the severe symptoms of type 1 diabetes (lethargy, depression, extreme thirst, urination every 45 minutes, metallic taste in mouth, extreme sleepiness) did indeed come about in a matter of days – but I had been noticing some odd symptoms for over a decade prior to my diagnosis.
My hope for this post is to educate people about the early symptoms that I had been shrugging-off in case they are having a similar experience. Due to the delay in my diagnosis, by the time I arrived in the doctor’s office, I had developed Stage 2 Chronic Kidney Disease, minor Diabetic Retinopathy (eye damage), Moderate Acid reflux and Gastroparesis, and likely damage to my heart and all of my blood vessels. 2 The sooner you diagnose developing T1D, the better your chances are at slowing the progression of the disease; this could result in better long term outcomes. 3
First Indications
My first inklings that I may have had a problem with my blood glucose occurred in my mid 20s. I would be on a bike ride – usually at the very beginning of a ride, and I would suddenly feel shaky, dizzy, panicked and extremely hungry (for sugar). All I knew was that eating something sweet would fix this problem in about 15 minutes. While I was feeling this way, it was impossible for me to pedal any further; my lips would be tingling and numb and my riding buddies would stop and wait for me. Usually, I’d be at the front of the group before it started, so by the time the last people in the group caught up, I’d be getting better – making the problem somewhat transparent. Over time, I realized what would trigger this phenomenon: Eating something like pancakes or bread about 1 hour prior to the start of the activity – and then driving in a car – would invariably result in this pattern of events. Oddly, eating something with a little fat and protein (like a granola bar) before the ride would not have the same effect.4
Around that time, I mentioned this issue to a friend who was a Certified Diabetes Educator (CDE) because I knew that this had something to do with blood sugar. Right away, she said,
“That could be diabetes.”
I laughed at her because it seemed like she thought everything was related to diabetes given her job. Besides, I figured that I was in the clear on both types of diabetes. I thought that you couldn’t get Type 1 (formerly called juvenile onset diabetes) once you were older than about 12. Also, I was very thin, exercised every day and ate a healthy, mostly vegetarian diet, so I figured that I was also exempt from Type 2 diabetes. Finally, I was having LOW blood sugars, and I thought:
“Isn’t diabetes HIGH blood sugars?”
I easily dismissed her comments, and went on with my life. Little did I know: I was wrong about everything – even on the possible types of diabetes (there are many more than just “type 1” and “type 2”).
What about Family History?
About the only thing that I took seriously from her comment was my family history. At the time, all I knew was that my dad had type 2 diabetes and he had to inject insulin.5 Years before, my mom was diagnosed with diabetes and given a blood sugar meter. Shortly after her diagnosis, I had even tested myself with her meter when I felt shaky a couple of times (getting readings of about 72mg/dL). She only used the meter for about 1 week before she gave up on it, but every reading in the memory for that week was over 300mg/dL. I knew that was high, but I didn’t know how serious that was. At the time, I assumed that diabetes was no big deal. You had some more sugar in your blood and you just kept on living – like she did.
A couple years later, my mom passed away from kidney failure. During the last 6 months of her life, she was in and out of the hospital a lot, and had even fallen into a coma that lasted over a week. We assumed that she died from alcoholism; every time I took her to the hospital, they mentioned concerns about her alcohol consumption, and NOT ONCE did they ever mention her blood glucose. It never occurred to me at the time to even think about her blood glucose, but now I know that persistent blood sugars over 300mg/dL can quickly be devastating to the kidneys and other organs. I assume she had been living with glucose levels that high for several years considering the one-week history I found in her blood glucose meter. I also now know that dry alcohol can temporarily reduce blood sugar (sometimes dramatically). I wonder if alcohol made her feel better partly because it temporarily brought her blood sugars closer to a normal range?
I completely ignored this family history because I incorrectly made the assumption that my mom and dad “didn’t take care of themselves.” They both drank alcohol, and neither one of them exercised. As far as I could tell, they both ate healthy diets – so I incorrectly assumed that type 2 diabetes was ultimately the plague of people who didn’t exercise.
Blaming my health problems on exercise
As time went on, I kind of forgot about my hypoglycemic episodes at the start of bike rides. On one hand, I knew how to prevent it (don’t eat certain foods & sit around 1 hour before a bike ride). On the other hand, they just stopped occurring. During this period, though, other strange things were happening to my body. I would notice that when I sat at my desk at work, I would need to get up and go to the bathroom a lot more frequently than my coworkers. Also, I’d always be really thirsty when sitting at my desk. I’d get up frequently to use the bathroom or get something to drink (water or (fortunately) diet soda). I was a bit embarrassed because I felt as if these frequent interruptions were hindering my efficiency at work. I also wondered how other people could go so long without bathroom breaks. The odd thing was that all of the thirst and bathroom breaks would go away as soon as I started exercising.6.
I used to keep a daily journal, and in looking back to when I was in my late 20s, I had written “diabetes?” in my journal after looking up my symptoms online. Of course I dismissed that… and now I was starting to have other health problems: A pain in my gut as well as an arrhythmia in my heart. Over time, I made a couple of visits to the doctor for these two issues. I did not have a very good doctor: When I told him where I was having the pain in the gut, he said, “You have acid reflux.” I asked, “but how can you know without doing any tests?” He said, “I know because I have it too.” I couldn’t believe he was a real doctor, and I insisted on getting tested. He reluctantly ordered an “Upper GI with barium sulfate,” and sure enough, the test revealed that I had acid reflux. After I was diagnosed with type 1 diabetes, I did more research and learned that long term, poorly controlled diabetes can cause a condition called “gastroparesis”. Gastroparesis is caused when diabetes damages the vagus nerve impairing the emptying of the stomach. When you lie down to go to bed, your stomach is still full of food, and it can reflux back into the esophagus. By the way, he never tested my blood sugar. In fact, in all 10 years of being with this doctor, I never had any blood tests. He sent me home with some Prilosec which I tried for a couple days and then discarded because they made me feel quite ill.
The thirst / bathroom trips continued, and I kept assuming this odd issue was due to my vigorous exercise. I exercised more than most people I knew – but not quite as much as a top level pro athlete. I assumed that pro-athletes also dealt with feeling lousy whenever they weren’t exercising. As time went on, I noted that I HAD to exercise to feel normal. If I skipped even 1 day of vigorous exercise, my entire body would ache as if I had the flu. I’d feel slightly feverish, lethargic, and have a slight metallic taste in my mouth. I’d ask my friends who exercised a lot:
“Does your entire body ache and feel feverish when you DON’T exercise?”
The answer would always be, “no,” so I just assumed that maybe I was exercising more or harder than they were – and that was why things were different.
My wife and I would sometimes go on road trips, which required me being immobile in a car for long periods of time. It began to become more and more obvious that if I drank any liquid while not exercising, I’d have to immediately go to the bathroom. She would ask why I didn’t plan ahead for bathroom stops, not understanding how quickly this came on. I now know that due to a lack of insulin, the metallic taste in my mouth and the flu like aches were being caused by acidic ketones in my blood. My body was becoming less able to use glucose due to the shortage of insulin – and being forced to use fat instead. The ketones were a byproduct of fat burning on overdrive.
Constant hunger… with no weight gain
Something else unusual I noticed was how much I was eating. From my early 20s until I got my diagnosis at 39, I had a running joke that I would “pre-eat” before going to a restaurant. The normal scenario was this: I’d eat an entire meal before going out to eat at a restaurant (for fear of tiny restaurant portions). At the restaurant, I’d eat my entire meal and still be hungry. After everyone was done, I’d ask if I could eat all of their leftover food as well, which I did. Once I got home, I’d usually be so hungry that I’d follow up with more food – often an entire pint of ice cream. I assumed that all this hunger and eating was because of my exercise. After all, I never gained weight – and my subcutaneous body fat seemed to be particularly low – no matter how much I ate. I found it odd that I could eat so much more food than my athletic friends – who ate FAR less than me. I assumed they were eating in secret. I joked with one of my friends that he was like a “Toyota Prius” and I was like an RV pulling a trailer in terms of fuel economy.
Unbelievably, this all went on for a decade and a half. I kept feeling lousy whenever I wasn’t exercising, I would eat tons and tons of food, I would frequently do internet searches for “chronic dehydration”, and I chalked all this up to my exercise routine. I often quipped to my wife:
“If I feel this bad in my 30s, I don’t think I can handle being in my 90s.”
My Pancreatic beta cells give the last gasp
In 2016, I had several additional health setbacks: I got two back-to-back intestinal infections while traveling in Peru. Although I partially recovered from both illnesses, it was obvious that a deep hole had been dug in my health. I pushed through the rest of the Peru bike tour riding a heavily loaded tandem on pure grit and passion, but by this point, my body was clearly falling apart.
Finally, 3 months after returning from Peru, I got well past my renal threshold for glucose – and stayed there. There is a very specific day that this happened, so if one were to ignore all the prior events, they would think that I got type 1 diabetes on that very day. Starting on that day, I was peeing at least once per hour. I felt beaten down; exhausted. I could barely ride my bike, and some deep depression had set in. I was losing 1.5 pounds of body weight per day. All I felt like doing was sleeping. I made a doctor appointment, and for the first time in over a decade, got some blood tests. I was still in denial that I might have “diabetes mellitus.” I had learned about “diabetes insipidus” online (this is where your body has trouble regulating how it handles fluids; it is unrelated to problems with the pancreas), and I assumed that I might have this condition. Before my blood test, the nurse said,
“Well, hopefully this is diabetes insipidus.”
Looking back, I think she already knew what was going on.
Diagnosis
The basic blood tests came back revealing a blood sugar of 300mg/dL. This meant “diabetes mellitus” and not “diabetes insipidus.” Since I was 39 years old, I assumed that I had somehow developed Type 2 diabetes. After all, I thought my dad has type 2 diabetes, and maybe my mom did too. I guessed that I needed to exercise more, and went to the gym the next day to start lifting weights – which made me feel even worse and caused my blood sugars to rocket into the mid 400mg/dL range. The following morning, I had another appointment with a different nurse who was a specialist in diabetes. When she walked in the room, she gasped,
“Oh God, you’re a type one!”
That was the very first thing she said – before even saying “hello”. I had lost so much weight and fat by this point, you could see my veins protruding from my skin all over my body. Regretfully, I had delayed visiting a doctor for too many years. The consequence of that was years of suffering and damage to every cell in my body.

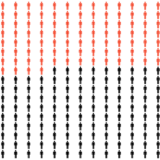
Most people associate “diabetes” with weight gain, but as TYPE 1 diabetes is developing, you actually start to lose all of your fat (as shown in this picture). This is because with TYPE ONE diabetes, your body cannot produce enough insulin – and insulin is what helps your body store food energy as fat. Without enough insulin, you actually excrete many of the calories you eat in your urine.
She prescribed a medication called “Lantus” (a long lasting form of insulin), and told me to start injecting 5 Units per day. She gave me permission to slowly titrate the dose upwards as needed. She also introduced me to all sorts of new technology (Continuous Glucose Monitors & Pumps) and said that I had picked the “best time in history” to get diagnosed with diabetes. She was right about that; even though diabetes is extremely difficult to manage, it is MUCH easier today than it was just 20 years ago. The technology appealed to me, as I like recording and interpreting data. It wasn’t until later that I would discover that the human body rarely functions in predictable ways, making technology less reliable than the more time consuming manual control.
I asked the nurse if we could make sure that I really had type 1 diabetes. She said that there were 4 or 5 antibodies that could be tested for verification… but she queried:
“what’s the point? The tests are expensive and the treatment is the same.”
I insisted, and she ordered the tests. I got them immediately – right before my very first injection of insulin (I didn’t want to confound the results with antibodies against injected insulin). The test results revealed that I had GAD antibodies that were too high to be measured on their scale – and very high IA-2 antibodies. Zinc Transporter and Insulin Antibodies were negative. Moreover, my c-peptide (an indirect measure of how much insulin your body can produce) was very low. This was an absolute diagnosis of classic “Type 1 diabetes,” which by definition is mediated by an autoimmune attack on the pancreatic beta cells. This differentiates the condition from Type 2 diabetes which is usually (but not always) caused by a relative overconsumption of calories.
Feeling good again
Within about 3 days of injecting the insulin, I began to feel better – like amazingly better. Because of the stark contrast to how I felt just a few days prior, I thought,
“I feel like I’m 16 again!”
I meant it. The depression quickly vanished in those few days, and after about a month, I managed to achieve almost normal blood sugars. I did this by eating almost no carbohydrate & using an “overdose” of Lantus. The nurse had not prescribed any insulin for meals, so it was impossible for me to eat any carbohydrates without shooting my blood sugar to the moon. I think that she had expected for me to have a “honeymoon” period. A honeymoon happens when people begin injecting insulin; the medication gives the pancreas a bit of a rest and it begins working again. I suspect that I already used up my “honeymoon” during those 15 years I spent feeling “off”. Just one month into injecting insulin, I had titrated up to almost the same equivalent Total Daily Dose that I now use 5 years later. Now, I use the Lantus 2x per day, along with a rapid acting insulin called Humalog several times a day for meals and making corrections.
My message to others
Having had this experience, I now regret not visiting the doctor for an annual checkup. It is likely that my condition would have been detected years earlier which could have saved a lot of damage to my body and long term health. Unfortunately, the most likely way this would have been detected is by having an “elevated fasting blood sugar.” It turns out that in the development of type one diabetes, fasting blood sugar is the last think to go. In other words, by the time this test reveals a problem, you’re already pretty late in the course of the development of T1D. My hope in publishing this post is that people learn that you can develop type 1 diabetes at any age. I hope that after reading this, my readers will be sure to get annual checkups for themselves as well as people who they care about. Diabetes is not the only condition that can be detected by annual screening. Please don’t be like me and avoid visiting the doctor for over a decade!
References & Footnotes
- Reference: Type 1 Diabetes: Etiology, Immunology, and Therapeutic Strategies, Tom L. Van Belle, Ken T. Coppieters, and Matthias G. Von Herrath, 2011, https://journals.physiology.org/doi/full/10.1152/physrev.00003.2010#_i20
- Note: I haven’t had this directly measured, but nerve and blood vessel damage is the underlying cause of all type 1 diabetes complications
- Reference: Staging Presymptomatic Type 1 Diabetes: A Scientific Statement of JDRF, the Endocrine Society, and the American Diabetes Association, Richard A. Insel et al., 2015, https://care.diabetesjournals.org/content/38/10/1964#sec-9
- Note: Although I never measured my blood sugars at the time, I now know that bread and pancakes very rapidly digest into a simple sugar called “glucose”. At the time, I did not consider that table sugar – which is used to sweeten packaged products such as granola bars – actually raises blood glucose MORE SLOWLY than some breads and pancakes. My theory is that my body was secreting a lot of insulin while I was sedentary during the drive to the bike ride, but as soon as I became active, there was too much insulin in my system (because insulin is MUCH MUCH more powerful during exercise). This abundance of insulin for the situation (exercise), is what was causing the severe drops in blood sugar
- Note: In a person with metabolic syndrome (often referred to as type 2 diabetes), insulin is usually not necessary for survival. In the early stages, most people can simply reduce their caloric intake to normalize blood sugars. This type of diabetes is what most people think of when they hear the word diabetes. Now that I know more about diabetes, I’m not certain that my dad has classic type 2 diabetes. Unfortunately, his doctors refuse to do the additional testing to determine the type.
- Note: Now that I know how insulin works in the body, I have a theory about this. I think that my body was making very small amounts of insulin that were not enough to maintain normal blood sugar when I was sedentary… but when you are exercising, your body needs almost no insulin. Since my body couldn’t produce much insulin, exercise was becoming my only escape into feeling normal



























Thank you Brian for the update and the story that is sure to motivate others to get the annual check up and annual blood tests. In addition, as you point out, even when you do see a doctor a person needs to advocate for themselves with regards to 2nd opinions, requesting testing, and possible health alternatives or medicine.
Thanks for another great and very educational post Brian.
I am so glad that you discovered you had T1D in time!